A hypertensive emergency is a condition in which elevated blood pressure results in target organ damage. The systems primarily involved include the central nervous system, the cardiovascular system, and the renal system. Malignant hypertension and accelerated hypertension are both hypertensive emergencies, with similar outcomes and therapies. In order to diagnose malignant hypertension, papilledema (as seen in the image below) must be present.
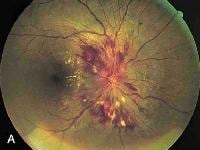 Papilledema. Note the swelling of the optic disc, with blurred margins.
Papilledema. Note the swelling of the optic disc, with blurred margins.
Up to 1% of patients with essential hypertension develop malignant hypertension, but the reason some patients develop malignant hypertension whereas others do not is unknown. The characteristic vascular lesion is fibrinoid necrosis of arterioles and small arteries, which causes the clinical manifestations of end-organ damage. Red blood cells are damaged as they flow through vessels obstructed by fibrin deposition, resulting in microangiopathic hemolytic anemia.
Another pathologic process is the dilatation of cerebral arteries following a breakthrough of the normal autoregulation of cerebral blood flow. Under normal conditions, cerebral blood flow is kept constant by cerebral vasoconstriction in response to increases in blood pressure. In patients without hypertension, flow is kept constant over a mean pressure of 60-120 mm Hg. In patients with hypertension, flow is constant over a mean pressure of 110-180 mm Hg because of arteriolar thickening. When blood pressure is raised above the upper limit of autoregulation, arterioles dilate. This results in hyperperfusion and cerebral edema, which cause the clinical manifestations of hypertensive encephalopathy.
Other causes of malignant hypertension include :
Any form of secondary hypertension; complications of pregnancy; use of cocaine, monoamine oxidase inhibitors (MAOIs), or oral contraceptives; and the withdrawal of alcohol, beta-blockers, or alpha-stimulants. Renal artery stenosis, pheochromocytoma (most pheochromocytomas can be localized using computed tomography (CT) scanning of the adrenals), aortic coarctation, and hyperaldosteronism are also secondary causes of hypertension. In addition, both hyperthyroidism and hypothyroidism can cause hypertension.
The following conditions should also be considered when making the diagnosis: stroke, intracranial mass, head injury, epilepsy or postictal state, connective-tissue disease (especially lupus with cerebral vasculitis), drug overdose or withdrawal, cocaine or amphetamine ingestion, acute anxiety, and thrombotic thrombocytopenic purpura.
Accelerated hypertension and hypertensive urgency
Accelerated hypertension is defined as a recent significant increase over baseline blood pressure that is associated with target organ damage. This is usually seen as vascular damage on funduscopic examination, such as flame-shaped hemorrhages or soft exudates, but without papilledema.
Hypertensive urgency must be distinguished from hypertensive emergency. Urgency is defined as severely elevated blood pressure (ie, systolic >220 mm Hg or diastolic >120 mm Hg) with no evidence of target organ damage.
Hypertensive emergencies require immediate therapy to decrease blood pressure within minutes to hours. In contrast, no evidence suggests a benefit from rapidly reducing blood pressure in patients with hypertensive urgency. In fact, such aggressive therapy may harm the patient, resulting in cardiac, renal, or cerebral hypoperfusion. This article discusses hypertensive emergency, but therapy for hypertensive urgency is discussed briefly.
Patient education
Patients must be taught an appropriate diet for long-term management, and upon discharge, patients should not only know the signs and symptoms that should prompt immediate notification of a physician but also know the proper dosing and adverse effects of their medications.

No comments:
Post a Comment