- Identification
- Name
- Age
- young age à more likely type 1 diabetes
- old à type 2 diabetes
- occupation à sedentary life style, drug compliance
- Presenting Complaint
- Polyuria, polydypsia, pholyphagia
- Lethargy, weakness, loss of weight
- Infection
- Complications
- History of presenting complaint
- When was he/she is diagnosed to be diabetic
- What were the symptoms he/she had
- What were the treatments given
- Adherence to treatments
- Problems with treatment/ side effects
- Was he/she advised regarding hypoglycemic attacks
- Was he/she advised about diet control
- Was he/she referred to eye clinic
- was he/she advised regarding foot care
- How many hospital admissions since then, for what illness, what was done
- Macrovascular complications
- Ischemic heart disease
- Perepheral vascular disease
- Leg ulcers
- Claudication
- Strokes/Transient ischemic attacks
- Microvascular complications
- Visual disturbances
- frothy urine, oliguria, red colored urine
- Nuropathies
- eripheral nuropathy - Loss of sensation, abnormal sensation, tingling of feet
- Mononuropathies - Symptoms of carpel tunnel syndrome/tarsal tunnel syndrome
- Autonomic nuropathy - impotence, gustatory sweating, urinary retension, incontenance, constipation, diarrhea, dizziness, recurrent nausea and vomiting
- Nuroglycopenic symptoms - impaired interlectual activity, diminished psychomotor skills, severe agitation, confusion, coma, epileptiform seizures
- Immunological complications
- Recurrent infections
- Urinary tract infections
- Balanitis
- pruritus vulvae
- Past Medical History
- strokes
- Ischemic heart disease
- Dyslipidemias
- Fits
- Bronchial asthma
- Strokes
- Past Surgical History
- Amputations
- Drug History
- antidiabetic drugs, side effects, compliance
- Allergic History
- Drug, food, laster allergies
- Family History
- Diabetes, premature heart diseases, Strokes, young deaths in first degree relatives
- Social History
- Educated up to
- Occupation
- Lives with
- Income
- Exercise
- Alcohol intake
- Smoking
- Nearest hospital
- Dietary history
- Regularity of meals
- Quality of content
- Fatty greasy food
- Fruit and vegetable content
- Sugar and sugary foods
- Salt
Showing posts with label Internal Medicine. Show all posts
Showing posts with label Internal Medicine. Show all posts
Monday, 14 April 2014
Diabetic melitus History Template
Tuesday, 4 February 2014
Tachycardia
Tachycardia
Tachycardia is a heart rate of more than 100 beats per minute. The heart normally beats at a rate of 60 to 100 times per minute, and the pulse (felt at the wrist, neck or elsewhere) matches the contractions of the heart's ventricles, the heart's two powerful lower chambers.
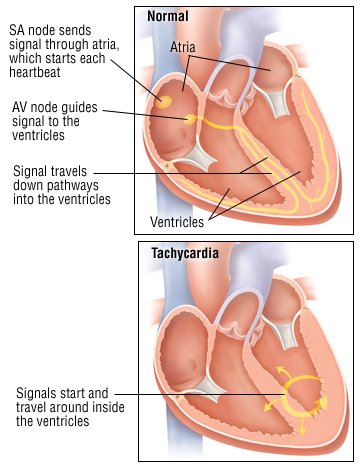 |
Tachycardia can be part of the body's normal response to anxiety, fever, rapid blood loss or strenuous exercise. It also can be caused by medical problems, such as an abnormally high level of thyroid hormones, called hyperthyroidism. In some people, tachycardia is the result of a cardiac arrhythmia (a heart-generated abnormality of heart rate or rhythm). Tachycardia can also be caused by lung problems, such as pneumonia or a blood clot in one of the lung's arteries.
In other cases, tachycardia can be a side effect of some foods and drinks, including coffee, tea, alcohol and chocolate; tobacco; or medication.
Symptoms
Symptoms of tachycardia can include:
- Dizziness, lightheadedness and fainting
- Fatigue (an abnormally tired feeling)
- Palpitations (awareness of a rapid heartbeat)
- Breathlessness
If tachycardia is caused by a medical illness, there will be additional symptoms that are specific to that illness. For example, people who have tachycardia caused by hyperthyroidism also can experience nervousness, insomnia, sweating, tremors and other symptoms related to high levels of thyroid hormones. Tachycardia caused by heart or lung disease often is accompanied by chest pain or shortness of breath or lightheadedness.
Diagnosis
Your doctor will ask you to describe your symptoms. He or she will review your personal medical history and potential causes of tachycardia, including lung disease, thyroid disorders, and medications. Your doctor will want to know if you have a family history of heart disease and cardiac arrhythmias.
During the physical examination, your doctor will check your heart rate and rhythm. Your doctor also will check for an enlarged heart, for heart murmurs (one sign of a heart valve problem), for abnormal lung sounds and for physical signs of thyroid abnormalities (enlarged thyroid gland, hand tremor and an abnormal protrusion of the eyes).
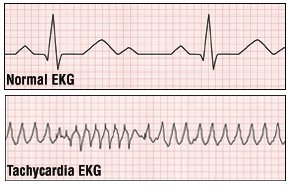
To further evaluate your tachycardia, your doctor will order an electrocardiogram (EKG). However, because some forms of tachycardia come and go, a one-time office EKG may be normal. If this is the case, you may need a test called ambulatory electrocardiography. For this test, you will wear a portable EKG machine called a Holter monitor for a period, usually for 24 hours. If symptoms occur infrequently, you may have to wear a monitor for much longer. You will be taught to press a button to record EKG readings when symptoms occur.
 |
Depending on the results of your physical examination, other tests may be necessary, such as blood tests to measure your red blood cell count and levels of thyroid hormones and an echocardiogram to see if there are any structural abnormalities of your heart. Sometimes, physicians do "electrophysiology testing," in which they insert special catheters within the heart to collect information on the patterns of the heart's electrical activities.
Expected Duration
How long tachycardia lasts depends on its cause. For example, tachycardia resulting from fever will go away when body temperature returns to normal. Tachycardia resulting from blood loss will end when the patient is stabilized with intravenous (IV) fluids and/or blood transfusions. Tachycardia resulting from hyperthyroidism or an adrenal gland tumor will go away when the disorder is treated. Tachycardia caused by medications or diet will go away quickly, usually within hours, when the chemical that is causing the problem is used up by the body or excreted in the urine. Tachycardia caused by cardiac problems can last a long time.
Prevention
Since tachycardia is usually a sign of some underlying medical problem, discovering and treating the cause is the best way to prevent recurrent tachycardia.
The first episode of an arrhythmia that causes a rapid heart beat usually cannot be prevented.
Treatment
The treatment of tachycardia depends on its cause. For example:
- Fever. Fever-related tachycardia can be treated with fever-reducing medications, such as acetaminophen (Tylenol) or ibuprofen (Advil, Motrin and others). If the fever is caused by a bacterial infection, antibiotics also may be needed.
- Blood loss. To treat blood loss, the patient first is stabilized with fluids given intravenously (into a vein) or blood transfusions. Then, the source of the bleeding is found and stitched, or corrected with surgery.
- Hyperthyroidism. Hyperthyroidism can be treated with antithyroid medications such as methimazole (Tapazole, generic versions). Alternative treatments include radioactive iodine, which destroys the thyroid with radiation, or removing most of the thyroid gland with a surgical procedure called subtotal thyroidectomy.
- Cardiac arrhythmias. The treatment depends on the cause of the arrhythmia. In some people, massaging the carotid sinus in the neck will stop the problem. Other people require medications such as digitalis (Lanoxin), beta-blockers, calcium channel blockers, or amiodarone (Cordarone, Pacerone, generic versions). Some patients respond only to radiofrequency catheter ablation, a procedure that destroys the area of abnormal heart tissue that is triggering the tachycardia. Other patients can be treated with electrical cardioversion, a procedure that delivers a timed electrical shock to the heart to restore normal heart rhythm.
- Lung disease. If the tachycardia is caused by a blood clot in the lungs, the usual treatment is medications that dissolve the clot and keep more clots from forming. Pneumonia or other lung problems can be treated with medications for those conditions.
Saturday, 25 January 2014
Compensatory Mechanisms Of Heart Failure
COMPENSATORY MECHANISMS
Several natural compensatory mechanisms are called into action in patients with heart failure that buffer the fall in cardiac output and help preserve sufficient blood pressure to perfuse vital organs. These compensations include (1) the Frank–Starling mechanism, (2) neurohormonal alterations, and (3) the development of ventricular hypertrophy and remodeling (Fig. 9.8).

Frank–Starling Mechanism
As shown in Figure 9.3, heart failure caused by impaired left ventricular contractile function causes a downward shift of the ventricular performance curve. Consequently, at a given preload, stroke volume is decreased compared with normal. The reduced stroke volume results in incomplete chamber emptying, so that the volume of blood that accumulates in the ventricle during diastole is higher than normal (see Fig. 9.3, point b). This increased stretch on the myofibers, acting via the Frank–Starling mechanism, induces a greater stroke volume on subsequent contraction, which helps to empty the enlarged left ventricle and preserve forward cardiac output (see Fig 9.8).
This beneficial compensatory mechanism has its limits, however. In the case of severe heart failure with marked depression of contractility, the curve may be nearly flat at higher diastolic volumes, reducing the augmentation of cardiac output achieved by the increased chamber filling. Concurrently in such a circumstance, marked elevation of the end-diastolic volume and pressure (which is transmitted retrograde to the left atrium, pulmonary veins, and capillaries) may result in pulmonary congestion and edema (see Fig. 9.3, point c).
Neurohormonal Alterations
Several important neurohormonal compensatory mechanisms are activated in heart failure in response to the decreased cardiac output (Fig. 9.9). Three of the most important involve (1) the adrenergic nervous system, (2) the renin–angiotensin–aldosterone system, and (3) increased production of antidiuretic hormone (ADH). In part, these mechanisms serve to increase systemic vascular resistance, which helps to maintain arterial perfusion to vital organs, even in the setting of a reduced cardiac output. That is, because blood pressure (BP) is equal to the product of cardiac output (CO) and total peripheral resistance (TPR), a rise in TPR induced by these compensatory mechanisms can nearly balance the fall in CO and, in the early stages of heart failure, maintain fairly normal BP. In addition, neurohormonal activation results in salt and water retention, which in turn increases intravascular volume and left ventricular preload, maximizing stroke volume via the Frank–Starling mechanism.
a rise in TPR induced by these compensatory mechanisms can nearly balance the fall in CO and, in the early stages of heart failure, maintain fairly normal BP. In addition, neurohormonal activation results in salt and water retention, which in turn increases intravascular volume and left ventricular preload, maximizing stroke volume via the Frank–Starling mechanism.
 a rise in TPR induced by these compensatory mechanisms can nearly balance the fall in CO and, in the early stages of heart failure, maintain fairly normal BP. In addition, neurohormonal activation results in salt and water retention, which in turn increases intravascular volume and left ventricular preload, maximizing stroke volume via the Frank–Starling mechanism.
a rise in TPR induced by these compensatory mechanisms can nearly balance the fall in CO and, in the early stages of heart failure, maintain fairly normal BP. In addition, neurohormonal activation results in salt and water retention, which in turn increases intravascular volume and left ventricular preload, maximizing stroke volume via the Frank–Starling mechanism.
Although the acute effects of neurohormonal stimulation are compensatory and beneficial, chronic activation of these mechanisms often ultimately proves deleterious to the failing heart and contributes to a progressive downhill course, as described later.
Adrenergic Nervous System
The fall in cardiac output in heart failure is sensed by baroreceptors in the carotid sinus and aortic arch. These receptors decrease their rate of firing in proportion to the fall in BP, and the signal is transmitted by the 9th and 10th cranial nerves to the cardiovascular control center in the medulla. As a result, sympathetic outflow to the heart and peripheral circulation is increased, and parasympathetic tone is diminished. There are three immediate consequences (see Fig. 9.9): (1) an increase in heart rate, (2) augmentation of ventricular contractility, and (3) vasoconstriction caused by stimulation of α-receptors on the systemic veins and arteries.
The increased heart rate and ventricular contractility directly augment cardiac output (see Fig. 9.2). Vasoconstriction of the venous and arterial circulations is also initially beneficial. Venous constriction augments blood return to the heart, which increases preload and raises stroke volume through the Frank–Starling mechanism, as long as the ventricle is operating on the ascending portion of its ventricular performance curve. Arteriolar constriction increases the peripheral vascular resistance and therefore helps to maintain blood pressure (BP = CO × TPR). The regional distribution of α-receptors is such that during sympathetic stimulation, blood flow is redistributed to vital organs (e.g., heart and brain) at the expense of the skin, splanchnic viscera, and kidneys.
Renin–Angiotensin–Aldosterone System
This system is also activated early in patients with heart failure (see Fig. 9.9), mediated by increased renin release. The main stimuli for renin secretion from the juxtaglomerular cells of the kidney in heart failure patients include (1) decreased renal artery perfusion pressure secondary to low cardiac output, (2) decreased salt delivery to the macula densa of the kidney owing to alterations in intrarenal hemodynamics, and (3) direct stimulation of juxtaglomerular β2-receptors by the activated adrenergic nervous system.
Renin is an enzyme that cleaves circulating angiotensinogen to form angiotensin I, which is then rapidly cleaved by endothelial cell-bound angiotensin-converting enzyme (ACE) to form angiotensin II (AII), a potent vasoconstrictor (see Chapter 13). Increased AII constricts arterioles and raises total peripheral resistance, thereby serving to maintain systemic blood pressure. In addition, AII acts to increase intravascular volume by two mechanisms: (1) at the hypothalamus, it stimulates thirst and therefore water intake; and (2) at the adrenal cortex, it acts to increase aldosterone secretion. The latter hormone promotes sodium reabsorption from the distal convoluted tubule of the kidney into the circulation (see Chapter 17), serving to augment intravascular volume. The rise in intravascular volume increases left ventricular preload and thereby augments cardiac output via the Frank–Starling mechanism in patients on the ascending portion of the ventricular performance curve (see Fig. 9.3).
Antidiuretic Hormone
Secretion of this hormone (also termedvasopressin) by the posterior pituitary is increased in many patients with heart failure, presumably mediated through arterial baroreceptors, and by increased levels of AII. ADH contributes to increased intravascular volume because it promotes water retention in the distal nephron. The increased intravascular volume serves to augment left ventricular preload and cardiac output. ADH also appears to contribute to systemic vasoconstriction.
Although each of these neurohormonal alterations in heart failure is initiallybeneficial, continued activation ultimately proves harmful. For example, the increased circulating volume and augmented venous return to the heart may worsenengorgement of the lung vasculature, exacerbating congestive pulmonary symptoms. Furthermore, the elevated arteriolar resistance increases the afterload against which the failing left ventricle contracts and may therefore impair stroke volume and reduce cardiac output (see Fig. 9.9). In addition, the increased heart rate augments metabolic demand and can therefore further reduce the performance of the failing heart. Continuous sympathetic activation results in downregulation of cardiac β-adrenergic receptors and upregulation of inhibitory G proteins, contributing to a decrease in the myocardium’s sensitivity to circulating catecholamines and a reduced inotropic response.
Chronically elevated levels of AII and aldosterone have additional detrimental effects. They provoke the production of cytokines (small proteins that mediate cell–cell communication and immune responses), activate macrophages, and stimulate fibroblasts, resulting in fibrosis and adverse remodeling of the failing heart.
Because the undesired consequences of chronic neurohormonal activation eventually outweigh their benefits, much of today’s pharmacologic therapy of heart failure is designed to moderate these “compensatory” mechanisms, as examined later in the chapter.
Natriuretic Peptides
In contrast to the ultimately adverse consequences of the neurohormonal alterations described in the previous section, the natriuretic peptides are natural “beneficial” hormones secreted in heart failure in response to increased intracardiac pressures. The best studied of these are atrial natriuretic peptide (ANP) and B-type natriuretic peptide (BNP). ANP is stored in atrial cells and is released in response to atrial distention. BNP is not detected in normal hearts but is produced when ventricular myocardium is subjected to hemodynamic stress (e.g., in heart failure or during myocardial infarction). Recent studies have shown a close relationship between serum BNP levels and the clinical severity of heart failure.
Actions of the natriuretic peptides are mediated by specific natriuretic receptors and are largely opposite to those of the other hormone systems activated in heart failure. They result in excretion of sodium and water, vasodilatation, inhibition of renin secretion, and antagonism of the effects of AII on aldosterone and vasopressin levels. Although these effects are beneficial to patients with heart failure, they are usually not sufficient to fully counteract the vasoconstriction and volume-retaining effects of the other activated hormonal systems.
Other Peptides
Among other peptides that are generated in heart failure is endothelin-1, a potent vasoconstrictor, derived from endothelial cells lining the vasculature (see Chapter 6). In patients with heart failure, the plasma concentration of endothelin-1 correlates with disease severity and adverse outcomes. Drugs designed to inhibit endothelin receptors (and therefore blunt adverse vasoconstriction) improve LV function in heart failure patients, but long-term clinical benefits have not been demonstrated.
Ventricular Hypertrophy and Remodeling
Ventricular hypertrophy and remodeling are important compensatory processes that develop over time in response to hemodynamic burdens. Wall stress (as defined earlier) is often increased in developing heart failure because of either LV dilatation (increased chamber radius) or the need to generate high systolic pressures to overcome excessive afterload (e.g., in aortic stenosis or hypertension). A sustained increase in wall stress (along with neurohormonal and cytokine alterations) stimulates the development of myocardial hypertrophy and deposition of extracellular matrix. This increased mass of muscle fibers serves as a compensatory mechanism that helps to maintain contractile force andcounteracts the elevated ventricular wall stress (recall that wall thickness is in the denominator of the Laplace wall stress formula). However, because of the increased stiffness of the hypertrophied wall, these benefits come at the expense of higher-than-normal diastolic ventricular pressures, which are transmitted to the left atrium and pulmonary vasculature (see Fig. 9.8).
The pattern of compensatory hypertrophy and remodeling that develops depends on whether the ventricle is subjected to chronic volume or pressure overload. Chronic chamber dilatation owing to volume overload (e.g., chronic mitral or aortic regurgitation) results in the synthesis of new sarcomeres in series with the old, causing the myocytes to elongate. The radius of the ventricular chamber therefore enlarges, doing so in proportion to the increase in wall thickness, and is termedeccentric hypertrophy. Chronic pressureoverload (e.g., caused by hypertension or aortic stenosis) results in the synthesis of new sarcomeres in parallel with the old (i.e., the myocytes thicken), termed concentric hypertrophy. In this situation, the wall thickness increases without proportional chamber dilatation, and wall stress may therefore be reduced substantially.
Such hypertrophy and remodeling help to reduce wall stress and maintain contractile force, but ultimately, ventricular function may decline, allowing the chamber to dilate out of proportion to wall thickness. When this occurs, the excessive hemodynamic burden on the contractile units produces a downward spiral of deterioration with progressive heart failure symptomatology.
Friday, 24 January 2014
Medical Mnemonics
simply means "memory aid".

Head & Neck
CRANIAL NERVES: I-Optic, II-Olfactory, III-Oculomotor, IV-Trochlear, V-Trigeminal, VI-Abducens, VII-Facial, VIII-Acoustic (Vestibulocochlear), IX-Glossophrayngeal, X-Vagus, XI-Spinal Accessory, XII-Hypoglossal
On Old Olympus Towering Tops, A Finn And German Viewed Some Hops (older and cleaner)
Oh Oh Oh To Touch And Feel A Girls Vagina And Hymen (newer and, well ...)
Which cranial nerve is Sensory, Motor, or Both- Some Say Marry Money, But My Brother Says Big Breasts Matter More
BRANCHES OF FACIAL NERVE: Temporal, Zygomatic, Buccal, Mandibular, Cervical
Ten Zebras Beat My Cock
Two Zulus buggered my cat –(for the sicker, amongst you!)
You have I nose. You have II eyes. (I - Olfactory; II -- Optic)
Standing Room Only -Exit of branches of trigeminal nerve from the skull S
V1 -Superior orbital fissure, V2 -foramen Rotundum, V3 -foramen Ovale
For the order of nerves that pass through the superior orbital fissure:
"Lazy French Tarts Lie Naked in Anticipation."
(Lacrimal, Frontal, Trochlear, Lateral, Nosociliary, Internal,
Abducens)
2 Muscle of mastication- Lateral Lowers- lateral pterygoid is the one that opens the jaw
4 Muscles of Mastication MTPP( which couldbe read as "Empty Peepee") -masseter, temporal, lateral and medial pterygoids --
Arteries as they come off the external carotid:
Superior thyroid, Ascending pharyngeal, Lingual, Facial, Occipital, Post Auricular, Superficial temporal, Maxillary
Some Anatomists Like Fucking, Others Prefer S & M
Some Angry Lady Figured out PMS
Innervation of Extraocularmotor Muscles:LR6 SO4 3
LR6--Lateral rectus--> VI abductens
SO4--Superior Oblique--> IV Trochlear
3--The remaining 4 eyeball movers = III Oculomotor
ABC'S of the aortic arch!
Aortic arch gives off the Bracheiocephalic trunk,
the left Common Carotid, and the left
Subclavian artery
BRACHIAL PLEXUS: Roots, Trunks, Divisions, Cords, Branches
Robert Taylor Drinks Cold Beer.
CERVICAL SPINAL NERVES:
c345 keeps the phrenic alive (innervation of phrenic nerve) c345 keep the diaphragm alive (innervation of diaphragm)
c5-6-7 raise your arms to heaven (nerve roots of long thoracic nerve innervate serratus anterior)
Cranial Bones
Annoying, aren't they?
The cranial bones are the PEST OF 6...
Parietal, Ethmoid,Sphenoid,Temporal,Occipital,Frontal- 6 ? (6-the number of bones!)
( another one) Old People From Texas Eat Spiders.
LOCATION OF THORACIC DUCT: The duck is between two gooses (duck = thoracic duct) 2 gooses = azyGOUS and esophaGOUS
Cartilages of the Larynx - There are 4 cartilages in the larynx whose initial letters are TEAC (also the brandname of a home stereo).
Thyroid, Epiglottis, Arytenoid, Cricoid
Abdomen-Pelvis
INNERVATION OF PENIS:
Parasympathetic puts it up; sympathetic spurts it out
Point , Shoot, Score! (erection, emmision ,ejaculation) Parasympathetic, Sympathetic , Somatomotor
"S2, 3, 4 keep the penis off the floor" Innervation of the penis by branches of the pudental nerve, derived from spinal cord levels S2-4
Structures perforating the esophagus
"At T8 you see, perforates the IVC" (inferior Vena Cava)
the "EsoVagus" pierce T10 (esophagus, vagus nerve)
T12 - red, white and blue (aorta,thoracic duct,azygous vein)
Femoral Sheath (lateral to medial) order of things in thigh -NAVEL
Nerve, Artery, Vein, Empty, Space, Lymphatics
Radial n. innervates the BEST!!!!
Brachioradialis
Extensors
Supinator
Triceps
Course of Ureters
Water runs under the bridge (uterine a. and ductus deferens)
Carotid Sheath-- VAN
Internal Jugular Vein
Common carotid Artery
Vagus Nerve
Dermatomes
C3 is a high turtleneck shirt
T4 is at the nipple
L1 is at the inguinal ligament (or L1 is IL -Inguinal ligament)
Randy Travis Drinks Cold Beer--Brachial plexus
Robert Taylor Drinks Cold Beer
Roots, Trunks, Divisions, Cords, Branches
Bones of the wrist -Scaphoid, Lunate, Triquetrum, Pisiform, Trapezium,
Trapezoid, Capitate, Hamate
1. Slowly Lower Tilly's Pants To The Curly Hairs
2. Swifty Lower Tilly's Pants to try coitus here. (the risque version)
3.Scared Lovers Try Positions That They Can't Handle. (Classic version)
Pelvic Diaphragm
PICOLO(A) -Posterior to anterior
PIriformis
COccygeus
Levator Ani
Pelvic Splanchic-Parasympathetic
Sacral Splanchic-Sympathetic
Armies travel over bridges, the Navy travels under.
(Bridge is the ligament...reference to suprascapular artery and nerve.)
Pad, dab. Dorsal ABduct...Palmar ADduct...interosseous muscles of hand/foot.
Layers of the epidermis-Germinativum or Basale, Spinosum, Granulosum, Lucidum, Corneum
Grandpa Shagging Grandma's Love Child.
Limbic System- the 5 F’s- Feeding, Fighting, Feeling, Flight and Fucking
The 5 sphincters found in the Alimentary Canal are APE OIL:
Anal, Pyloric, Lower Esophogeal, Oddi, and Ileocecum.
Sally Thompson Loves Sex And Pot pie. The branches of the Axillary Artery are: Superior Thoracic, Thoracoacromial, Lateral Thoracic, Subscapular, Anterior Circumflex Humeral, Posterior Circumflex Humeral, and Profunda Brachii.
TIRE- four abdominal muscles -- transversus, internal oblique, rectus abdominus, and external oblique
GFR -Layers of the adrenal:-- Glomerular, Fascicular, Reticular
In the Phasted State Phosphorylate
Phosphorylation cascade active when blood glucose low.
Exons expressed, Introns in the trash--DNA expression into mature mRNA
Pyrimidines are CUT from purines.
Pyrimidines are Cytosine, Uracil, Thiamine and are one ring structures.
Purines are double ring structures.
Amino Acids:The ten essential amino acids:
"These Ten Valuable Amino Acids Have Long Preserved Life In
Man."
(Threonine, Tryptophan, Valine, Arginine, Histidine, Lysine,
Phenylalanine, Leucine, Isoleucine, Methionine)
INsulin gets sugar INto cells- (Excess sugar is removed via urine.The Romans noticed bees attracted to the urine of diabetics and coined the term "diabetes" to describe the overflow of sugar.)
GOAT FLAP- Eight hormones: Growth hormone, Oxytocin, Adenocorticotropin, Thyroid stimulating hormone, Follicle stimulating hormone, Leutinizing hormone (interstitial cell stimulating hormone in males), Anti-diruetic(Vasopressin), and Prolactin
(shhhh.... also Melatonin!)
Morphine excites men, but sedates cats.
One heart two lungs--beta receptor activity
Beta-1 primarily on heart; airway is beta-2 receptors
Meckel’s diverticulum- rule of 2’s
2 inches long,
2 feet from the ileocecal valve,
2% of the population
commonlly presents in the first 2 years of life
may contain 2 types of epithelial tissue
Pheochromocytoma-rule of 10s:
10% malignant
10% Bilateral
10% extraadrenal
10% calcified
10% children
10% familial
* discussed 10 times more often than actually seen
Aphasia
"BROKen aphasia" (Broca’s aphasia-broken speech)
"Wordys aphasia" (Wernicke’s aphasia- wordy, but making no sense)
GET SMASH'D--Causes of Acute pancreatitis
Gallstones, Ethanol, Trauma, Steroids, Mumps, Autoimmune(PAN), Scorpion bites, Hyperlipidemia, Drugs(azathioprine, diuretics)
(Multiple endocrine neoplasia) Each of the MENs is a
disease of three or two letters plus a feature.
"MEN I" is a disease of the 3 Ps (pituitary, parathyroid and pancreas)
plus adrenal cortex.
"MEN II " is a disease of the two Cs (carcinoma of the thyroid and
catacholamines [pheochromocytoma]) plus parathyroid for MEN IIa or
mucocutaneous neuromas for MEN IIb (aka MEN III).
Acute pneumonia caused by Pyogenic bacteria--PMN infiltrate
Acute pneumonia caused by Miscellaneous microbes --Mononuclear infiltrate
Takayasu's diz = pulseless diz, therefore when you have
Takayasu's, I can't Tak'a yu pulse.
Argyll-Robertson Pupil--syphilitic pupil (AKA "Prostitute's pupil" - Accommodates, but doesn't react )
Accommodation reflex present, Pupillary reflex absent
CAGE--alcohol use screening
1. Have you ever felt it necessary to CUT DOWN on your drinking?
2. Has anyone ever told you they were ANNOYED by your drinking?
3. Have you ever felt GUILTY about your drinking?
4. Have you ever felt the need to have a drink in the morning for an EYE OPENER?
P-Q-R-S-T--eliciting and HPI and exploring symptoms
P--palliative or provocative factors for the pain
Q--quality of pain(burning, stabbing, aching, etc.)
R--region of body affected
S--severity of pain(usually 1-10 scale)
T--timing of pain(eg.-after meals, in the morning, etc.)
The five W's--post-operative fever
Wind--pneumonia, atelectasis
Water--urinary tract infection
Wound--wound infections
Wonderdrugs--especially anesthesia
Walking--walking can help reduce deep vein thromboses and pulmonary embolus
ACID or "Anna Cycled Immediately Downhill"
classification of hypersensitivity reactions
Type I - Anaphylaxis
Type II - Cytotoxic-mediated
Type III - Immune-complex
Type IV - Delayed hypersensitivity
WBC Count:
"Never Let Momma Eat Beans(60, 30, 6, 3, 1)
Neutrophils 60%
Lymphocytes 30%
Monocytes 6%
Eosinophils 3%
Basophils 1%
A-P-G-A-R:
A - appearance (color)
P - pulse (heart rate)
G - grimmace (reflex, irritability)
A - activity (muscle tone)
R - respiratory effort
Predisposing Conditions for Pulmonary Embolism: TOM SCHREPFER
T--trauma
O--obesity
M--malignancy
S--surgery
C--cardiac disease
H--hospitalization
R--rest (bed-bound)
E--estrogen, pregnancy, post-partum
P--past hx
F--fracture
E--elderly
R--road trip
The 4 P's of arterial Occlusion: pain pallor pulselessness paresthesias
The 4 T's of Anterior Mediastinal Mass:Thyroid tumor,Thymoma,Teratoma, Terrible Lymphoma
Monday, 20 January 2014
NEMONIC for causes of CLUBBING>>>
the mnemonic is C.L.U.B.B.I.N.G, while the L has an extension of A.B.C.D.E.F
Cyanotic heart disease
Lung disease
Abscess
Bronchiectasis
Cystic Fibrosis
Dont say COPD
Empyema
Fibrosis
Ulcerative Collitis + Inflammatory Bowel Disease(Crohn's Disease)
Biliarty cirrhosis
Birth Defects
Infective Endocarditis
Neoplasm(eg. Lung cancer or mesothelioma)
Gastrointestinal malabsorption syndrome(Coeliac disease)
the mnemonic is C.L.U.B.B.I.N.G, while the L has an extension of A.B.C.D.E.F
Cyanotic heart disease
Lung disease
Abscess
Bronchiectasis
Cystic Fibrosis
Dont say COPD
Empyema
Fibrosis
Ulcerative Collitis + Inflammatory Bowel Disease(Crohn's Disease)
Biliarty cirrhosis
Birth Defects
Infective Endocarditis
Neoplasm(eg. Lung cancer or mesothelioma)
Gastrointestinal malabsorption syndrome(Coeliac disease)
Saturday, 11 January 2014
Clotting Factors
Clotting factors are substances in the blood that act in sequence to stop bleeding by forming a clot.
Here's a mnemonic to help you remember them ^___^
I Fibrinogen
II Prothrombin
III Tissue factor
IV Calcium
V Proaccelerin, Labile factor
VI Unassigned – Old name of Factor Va
VII Stable factor, proconvertin
VIII Antihemophilic factor A
IX Antihemophilic factor B or Christmas factor
X Stuart-Prower factor
XI Plasma thromboplastin antecedent
XII Hageman factor
XIII Fibrin-stabilizing factor
Mnemonics:
"Fresher's Party Tonight, Come Let's Sing And Call Seniors, Please Have Fun"
"Foolish People Try Climbing Long Slopes After Christmas, Some People Have Fallen"
"Fit Pants, Tight Collars, Loose American Shirts Are Cool Says Pretty Heroine Farah"
My favorite mnemonic is the pretty heroine one.. I drew it too :P
Sunglasses = Cool ;)
Here is how you draw the coagulation cascade:
Intrinsic pathway is activated bysubendothelial collagen.
Extrinsic pathway is activated by tissue thromboplastin.
Another mnemonic:
1972 WEPT
1972: Factors 10, 9, 7 & 2
W: Warfarin
E: Extrinsic
PT: Prothrombin Time
Factors X, IX, VII, II are Vitamin K dependent.
Warfarin acts on extrinsic pathway,prothrombin time used to check it.
If you know this, the other one is the other one.
Heparin acts on intrinsic pathway, partial thromboplastin time is used to check it.
Here is one for hemophilia.
Remember in hemophilia, bleeding time is normal, PTT is increased.
Here's a mnemonic to help you remember them ^___^
.jpeg) |
| Clotting factors mnemonic |
II Prothrombin
III Tissue factor
IV Calcium
V Proaccelerin, Labile factor
VI Unassigned – Old name of Factor Va
VII Stable factor, proconvertin
VIII Antihemophilic factor A
IX Antihemophilic factor B or Christmas factor
X Stuart-Prower factor
XI Plasma thromboplastin antecedent
XII Hageman factor
XIII Fibrin-stabilizing factor
Mnemonics:
"Fresher's Party Tonight, Come Let's Sing And Call Seniors, Please Have Fun"
"Foolish People Try Climbing Long Slopes After Christmas, Some People Have Fallen"
"Fit Pants, Tight Collars, Loose American Shirts Are Cool Says Pretty Heroine Farah"
My favorite mnemonic is the pretty heroine one.. I drew it too :P
Sunglasses = Cool ;)
Here is how you draw the coagulation cascade:
Intrinsic pathway is activated bysubendothelial collagen.
Extrinsic pathway is activated by tissue thromboplastin.
Another mnemonic:
1972 WEPT
1972: Factors 10, 9, 7 & 2
W: Warfarin
E: Extrinsic
PT: Prothrombin Time
Factors X, IX, VII, II are Vitamin K dependent.
Warfarin acts on extrinsic pathway,prothrombin time used to check it.
If you know this, the other one is the other one.
Heparin acts on intrinsic pathway, partial thromboplastin time is used to check it.
Here is one for hemophilia.
Remember in hemophilia, bleeding time is normal, PTT is increased.
Subscribe to:
Posts (Atom)





